Sepsis: Your Treatment
- Luz Silverio
- Jan 6, 2019
- 4 min read
This is part two in a three-part series regarding sepsis management.

Choices with fluids:
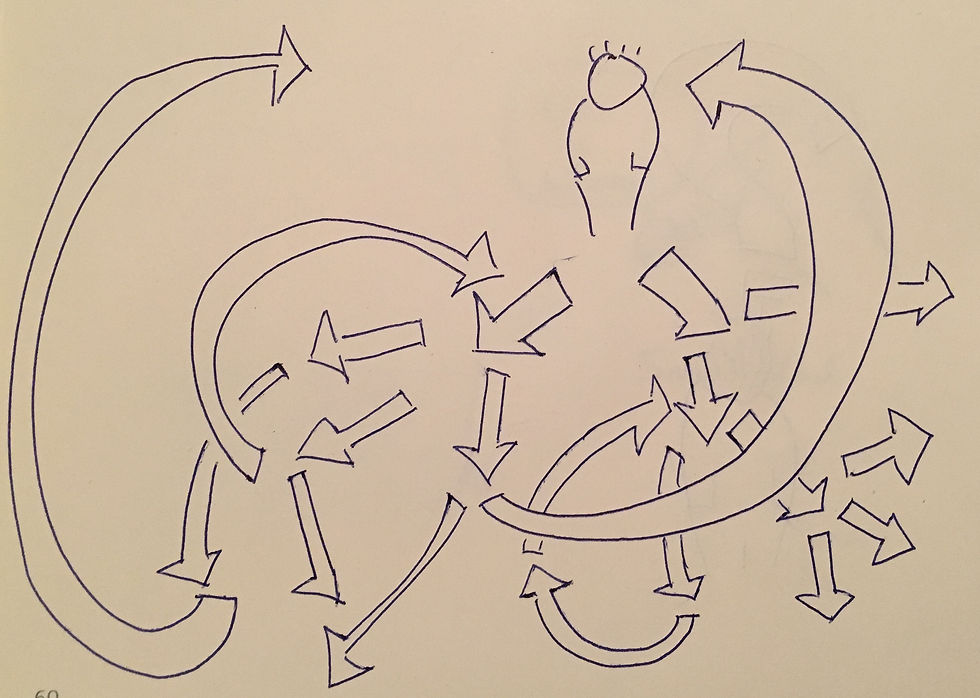
Current sepsis guidelines recommend a fluid bolus of 30cc/kg in the treatment of sepsis, to treat end-organ dysfunction or hypotension. But-- many of our patients have heart failure or kidney disease and are at significant risk for fluid overload. How do you deduce whether or not your patient will respond to that fluid bolus?
Historically, central venous pressure (CVP) monitoring was used to determine fluid responsiveness, and it's still recommended as one of the possible ways to assess for hemodynamic status in the CMS sepsis bundle. However, numerous studies have demonstrated that the CVP is essentially the same between fluid responsive and nonresponsive patients… That’s not to mention that a central line is required to measure it and pretty invasive.
Another invasive way to measure fluid responsiveness that has been demonstrated to work well is pulse pressure variation with respirations. If the patient is intubated and an arterial line is present, a significant pulse pressure variation can discriminate nonresponders from responders. There are some studies that show that in the setting of valsalva, pulse pressure variation works well to assess for fluid responsiveness even in patients who are breathing spontaneously, but this has not yet been externally validated.
In patients who are both spontaneously breathing and relatively line free, there are two tools at hand for assessing fluid responsiveness that have been demonstrated to have a reasonably good diagnostic accuracy.
Use the ultrasound to assess caval index of the inferior vena cava. To measure the caval index, use the cardiac or curvilinear probe. Measure the diameter of the IVC 3cm caudal to the junction of the IVC and the right atrium. Use M-mode to track changes in the diameter. The % change in diameter over the respiratory cycle is the caval index. A caval index of over 25% is 87% sensitive, 81% specific for measuring fluid responsiveness.
Alternatively, use a bioreactance measurement device (such as the NICOM) to assess for change in stroke volume with passive leg raise. A stroke volume increase of over 10% with 3 minutes of passive leg raise has an odds ratio of 9.5 for prediction of fluid responsiveness.
If you've decided that your patient is volume responsive, what fluid type should you use? Unless your patient has a significant acidosis, choosing something like normal saline should be fine for the first bolus, but there is some evidence that shows that increased normal saline is associated with increased mortality, and that balanced fluids (like LR or isolyte) is protective (OR 0.78, CI 0.964-0.993).
Lactated ringers is another good option. There has been some hesitation regarding lactated ringers in patients with sepsis because of a well-documented phenomenon in which the laboratory lactate values increase after a bolus of LR. This is probably happening because the lactate draw is in some proximity to the actively infusing LR, and not actually because of increasing systemic lactate. A recent study showed no increase in lactate when comparing patients receiving LR to NS, after a standard sepsis 30cc/kg bolus, when drawn from contralateral sites. If you do choose LR, make sure your nurse knows to draw that repeat lactate from somewhere else, to flush the IV vigorously with normal saline, or to wait a while after the infusion has stopped before drawing the lab.
Finally, isolyte or plasmalyte--these electrolyte-based fluids are more balanced for the human body, but also carry a hefty cost with them. They also may be difficult to get, depending on your practice setting.

Choices with antibiotics:
Current CMS guidelines require "blood cultures prior to antibiotics" but this doesn't necessarily come to fruition in the emergency department. Patients have difficult access and only one blood culture is obtained prior to antibiosis. And that's okay! CMS guidelines are met if one blood culture is obtained. In the setting of sepsis, blood cultures can be helpful in the determination of antibiotic coverage and duration of treatment, but this "blood cultures before antibiotics" recommendation does not mean that any patient that needs antibiotics also needs antibiotics. In the uncomplicated patient with community acquired pneumonia, the number needed to treat for cultures to affect treatment in a legitimate way is 250! In uncomplicated cellulitis, for example, blood cultures are often more likely to be false-positive for skin contamination flora than they are to actually diagnose the organism causing the infection.

In order to choose the appropriate antibiotics, the patient's reported allergies must be addressed. Approximately 10% of patients report allergies to penicillin, which could significantly alter therapy choices. Of these patients, only 10% of them have true allergies. in other words, true penicillin allergies occur in only approximately 1% of the population.
And if a reported penicillin allergy is causing a hesitance to give ceftriaxone, reconsider. The overall cross reactivity between reported “penicillin allergies” and cephalosporin allergies is a measly 1%. Even in patients with DOCUMENTED penicillin allergies their cross-reactivity with a cephalosporin is 2.5% Furthermore, 3rd and 4th generation cephalosporins (like) don’t even have the side chain that pen allergies are attributed to, so there is likely no cross-reactivity at all.
References:
Jalil BA, Cavallazzi R. Predicting fluid responsiveness: A review of literature and a guide for the clinician. Am J Emerg Med:36(2018)2093-2102.
Corl KA et al. Inferior vena cava collapsibility detects fluid responsiveness among breathing critically-ill patients. J Crit Care. 2017 Oct;41:130-137.
Duus N et al. The reliability and validity of passive leg raise and fluid bolus to assess fluid responsiveness in spontaneously breathing emergency department patients. J Crit Care. 2015 Feb;30(1):217
Zitek T et al. Does Intravenous Lactated Ringer’s Solution Raise Serum Lactate? J Emerg Med(2018)55;3:313-318.
Sethi M et al. Choice of resuscitative fluids and omrtality in emergency department patients with sepsis. Am J Emerg Med (2018)36;4, 625-629.
Long B, Koyfman A. Best Clinical Practice: Blood Culture Utility in the Emergency Department. J Emerg Med. 2016 Nov;51(5):529-539.
Raja AS, et al. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Ann Emerg Med. 2009 Jul;54(1):72-7.
CampagnaJD et al. The use of cephalosporins in penicillin-allergic patients: A literature review. J Emerg Med. 2012;42(5):612-20.
























Comments